CAR-T therapies, as well as up-and-coming T-cell engager (TCE) bispecifics, have been the buzz within hematologic circles for quite some time. TCEs and CAR-Ts are currently approved in both multiple myeloma (MM) and non-Hodgkins lymphoma (NHL). Each has its own advantages and disadvantages, with hematologists learning more each day about which approach is best, and it is still unclear which MOA will end up on top.
Recently, we had the opportunity to speak with a handful of leading physicians in the hem/onc space to get their input on this topic. In this article, we provide our thoughts on what the future could hold in the CAR-T and TCE space.
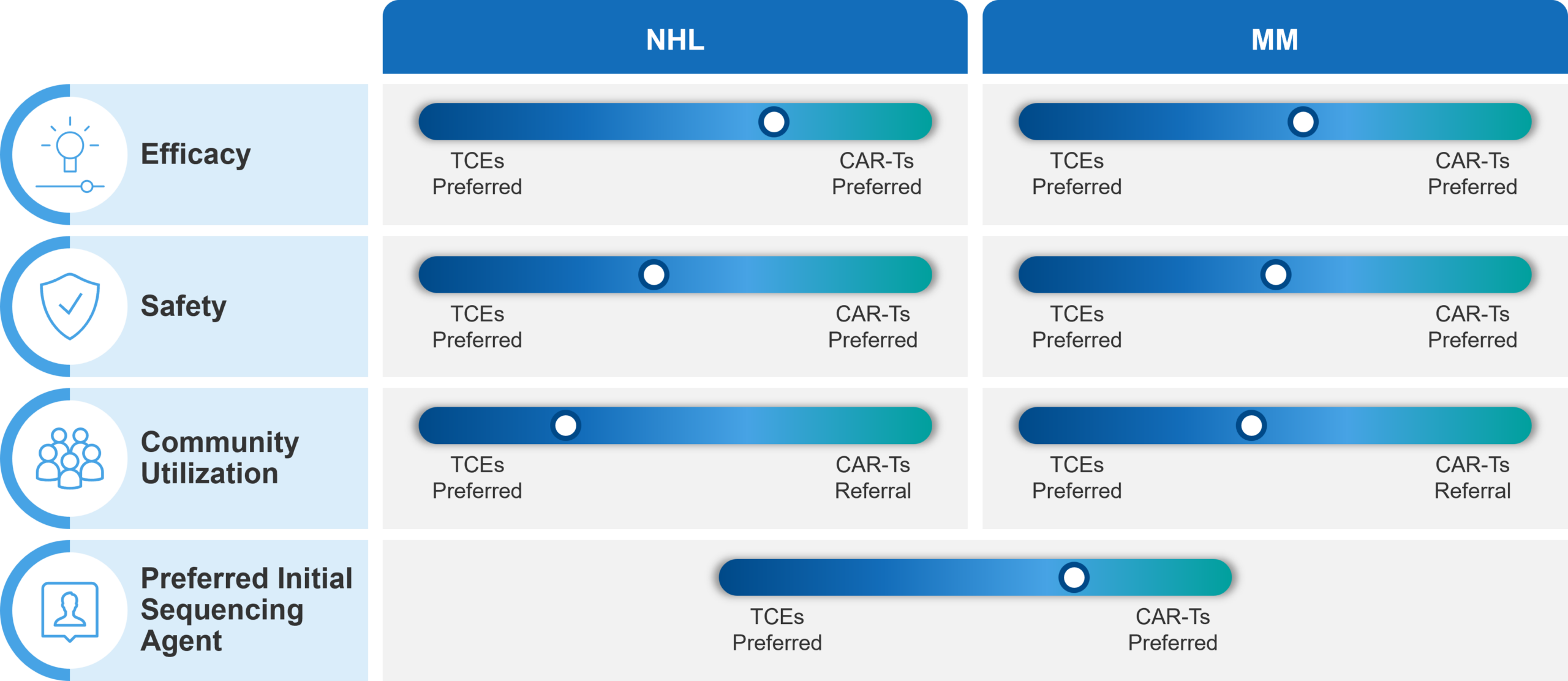
Efficacy:
In NHL, CAR-T and TCE complete response (CR) rates are viewed as comparable; However, CAR-T long term follow-up data and proven survival maintains CAR-T advantage.
When it comes to efficacy, CAR-Ts have been on the market longer, with long-term overall survival (OS) data that support the curative potential of the class in NHL. In our interviews, one physician noted that, “In terms of clinical efficacy, I’d rather see some long-term follow-up data on TCEs. With CAR-Ts, we now have five-plus year follow-ups in most pivotal studies. I think most of us, at least those who were involved with CAR-Ts from the start, still prefer them because of their potential to cure a subset of patients (although they still don’t cure a majority). Plus, we are not seeing relapses at the tail end. I’ve yet to see that for TCEs.”
On the other hand, TCEs have shown promising CR rates and initial durability of response, especially in non-aggressive lymphomas. However, the jury is still out on whether this will translate into “curative” potential similar to CAR-Ts. As one hematologist offered, “The TCE responses are holding up quite well, especially in indolent lymphoma, like mantle cell and follicular lymphoma. The OR (overall response) rates and CR rates are fairly comparable to those in the relapsed CAR-T setting. So, this is a good option because we know that less than 10% of the eligible patients for CAR-T actually get the therapy in this country for a variety of reasons.”
Safety:
Physicians believe that NHL TCEs are safer than MM TCEs; The risk of secondary malignancies with CAR-Ts is not viewed as a major barrier in the current treatment setting in heavily pretreated patients.
While physicians do not draw a direct comparison between the adverse event (AE) profile of CAR-Ts and TCEs, they do note that AE management with TCEs appears to vary based on tumor type. One physician states that, “… lymphoma TCEs are a bit safer than myeloma TCEs in terms of CRS (cytokine release syndrome). And the REMS requirements are not a factor. In fact, there is no REMS requirement at all. So that makes the execution quite easy for lymphoma doctors and community practices.”
The recent FDA announcement on its investigation of CAR-T-related secondary T-cell malignancies does not seem to have impacted the current safety perception of CAR-Ts. The physicians that we spoke to noted that currently CAR-Ts are used in the relapsed / refractory setting in both NHL and MM. In that setting, the risk of secondary malignancies might be viewed as acceptable, given the potential for a cure and limited treatment options.
However, CAR-Ts may receive more scrutiny regarding secondary malignancies as they move into earlier lines of treatment. In those situations, patients may benefit from long disease-free remission with existing conventional regimens that do not carry a similar risk.
Site of Care Dynamics:
Community physicians are getting increasingly more comfortable with TCE administration and AE management.
TCEs provide an off-the-shelf, readily available, and powerful option that democratizes treatment across different care settings and patient types. CAR-Ts, on the other hand, involve complex administration, but offer the benefit of a “one-and-done” treatment compared to repeated administrations of bispecific antibodies. This element gets even more attention in MM, where patients are often placed on treat-to-progression regimens, sometimes for years.
Currently, community physicians still refer MM and NHL patients to centers of excellence for additional consultation before making treatment decisions that may affect their eligibility for subsequent treatments. Despite the data limitations of relatively new TCEs, physicians note increased uptake and administration in the community setting. In particular, physicians indicate that they see this trend in the treatment of myeloma, a disease that is widely treated in the community setting. However, they indicate that this trend is more likely to increase among NHL treating physicians, given the favorable and manageable adverse event profile of CD19 TCEs.
In our interviews, one physician shared that, “Community colleagues still prefer our opinion (CoE physicians) before pulling the trigger on a certain therapy…and we are still recommending CAR-Ts, at least for high-grade lymphoma. But I would say that in the next two or three years, they will not ask me before treating. In myeloma, I have already started to see community (large community practices) use bispecifics before they even refer patients to us. In reality, I’m even beginning to see the same thing happen for lymphoma. It’s just a matter of time.”
At launch there were concerns about community physicians’ willingness and ability to manage hospitalization and AE monitoring with TCEs. The KOLs that we spoke to indicated that these barriers to use are typically temporary and that community physicians will learn to adapt over time. For example, community physicians have become comfortable with administration of other therapies with similar requirements, such venetoclax (which requires hospitalization during step-up dosing) and daratumumab, which requires close monitoring for infusion reactions. One KOL added that, “There is always a learning curve. I remember the days when daratumumab came around for the first time and there was this huge education component around infusion-site reactions. I think community practices now have more comfort using immunotherapies.”
Sequencing:
Physicians are concerned with T-cell exhaustion post TCE treatment that may temper subsequent CAR-T treatment outcomes.
One of the key concerns expressed by KOLs is the lack of data to establish the best treatment sequence for TCEs and CAR-Ts. This point is critical in the treatment of MM, in which both CAR-Ts and TCEs aim at the same target: BCMA (B-cell maturation antigen). There is a concern that initial treatment with TCE would result in inferior responses to subsequent CAR-T treatment (performed with curative intent) because of potential:
- T-cell exhaustion due to hyper-stimulation
- Evolving resistance due to BCMA mutations or down-regulation
T-cell exhaustion following TCE treatment may also impair the effectiveness of subsequent TCE treatment, even if aimed at a different target, such as GPRC5. During our interviews, one KOL drove both points home: “What I don’t think is reasonable, at least with our insights so far, is to expect good responses to CAR-Ts post-TCEs. Also, what I think may be a challenge, even if you switch targets, is to expect a slam dunk with TCE after TCE because of T-cell exhaustion or fatigue.” Another added, “Once you have used a bispecific, the response for CAR-T is quite inferior.”
Figure 1: Current perceptions among physicians of TCEs vs. CAR-Ts in NHL and MM
Future Competition
The CAR-T vs. bispecific field is a rapidly evolving one. Looking to the future, we have a few predictions:
- Indolent lymphomas: TCEs are likely to have a strong value proposition, given their ease of use. Additionally, the risk of secondary malignancy from CAR-Ts is a significant disincentive for their use in less aggressive tumor types. We expect bispecifics to establish a strong foothold in indolent lymphomas.
- MM: CAR-Ts are likely to remain the preferred MOA, as TCE data in MM to date have not been as compelling.
- NHL: The future is less clear in NHL and the space is likely to remain hotly contested between the two MOAs until long-term TCE durability and sequencing data are available.
Coming Next
In part II, we’ll look ahead and explore the future treatment dynamics in the hem/onc space. For example, we’ll address the inevitable move to outpatient CAR-T administration, as well as moving these therapies to earlier in the treatment paradigm.
We’ll also expand our view, addressing the role of conventional therapies in MM, the role of stem cell transplantation in NHL, future trends in patient segmentation, and more. As with this article, we’ll supplement our thoughts with insights from leading hem/onc professionals who are currently treating patients and conducting research in these areas. Stay tuned!